What is a Rotator Cuff Tear?
The rotator cuff is a group of four tendons that surround and stabilize the shoulder joint, connecting the muscles of the upper arm to the shoulder blade. When a rotator cuff tear occurs–from acute trauma, repetitive stress, or degeneration over time–the tendon becomes separated from its attachment point on the bone. Rotator cuff tears are painful and cause weakness in the joint and limited shoulder mobility. Common symptoms of a tear include difficulty lifting your arm, a popping or crackling sensation in the shoulder, and pain both at rest and with movement.
Unfortunately, rotator cuff tears don’t heal on their own. If an untreated tear results in arthritis in the joint, patients often require shoulder replacement surgery, but for patients who still have shoulder function and haven’t developed arthritis, there is a less invasive treatment option called the Stryker InSpace Balloon.
What is the Stryker InSpace Balloon?
The Stryker InSpace Balloon is a medical device used to treat rotator cuff tears. It’s made of biocompatible material–a substance that can be implanted in the body and tolerated without damaging existing tissue. The balloon creates more space within the subacromial area–the space between the bone at the top of the shoulder and the ball of the shoulder–reducing compression and friction caused by the torn rotator cuff.
What’s involved in the procedure?
The Stryker InSpace Balloon is placed arthroscopically, using a small incision and the guidance of a camera to precisely place the deflated balloon in the subacromial space. The balloon is then inflated with a sterile saline solution, causing it to push the acromion away from the rotator cuff tendons. This reduces impingement on the injured tissues to restore function and alleviate pain.
The procedure is minimally invasive and performed on an outpatient basis. Recovery time varies, depending on the individual patient and the extent of the injury, and rehabilitation may include physical therapy to help restore strength and mobility in the shoulder.
How do I know if the Stryker InSpace Balloon can help me?
If you’re experiencing shoulder pain, or have been diagnosed with a rotator cuff tear, it’s important to consult with a shoulder specialist as soon as possible. The specialist will evaluate your injury and medical history, and may recommend the Stryker InSpace Balloon procedure as a treatment option.
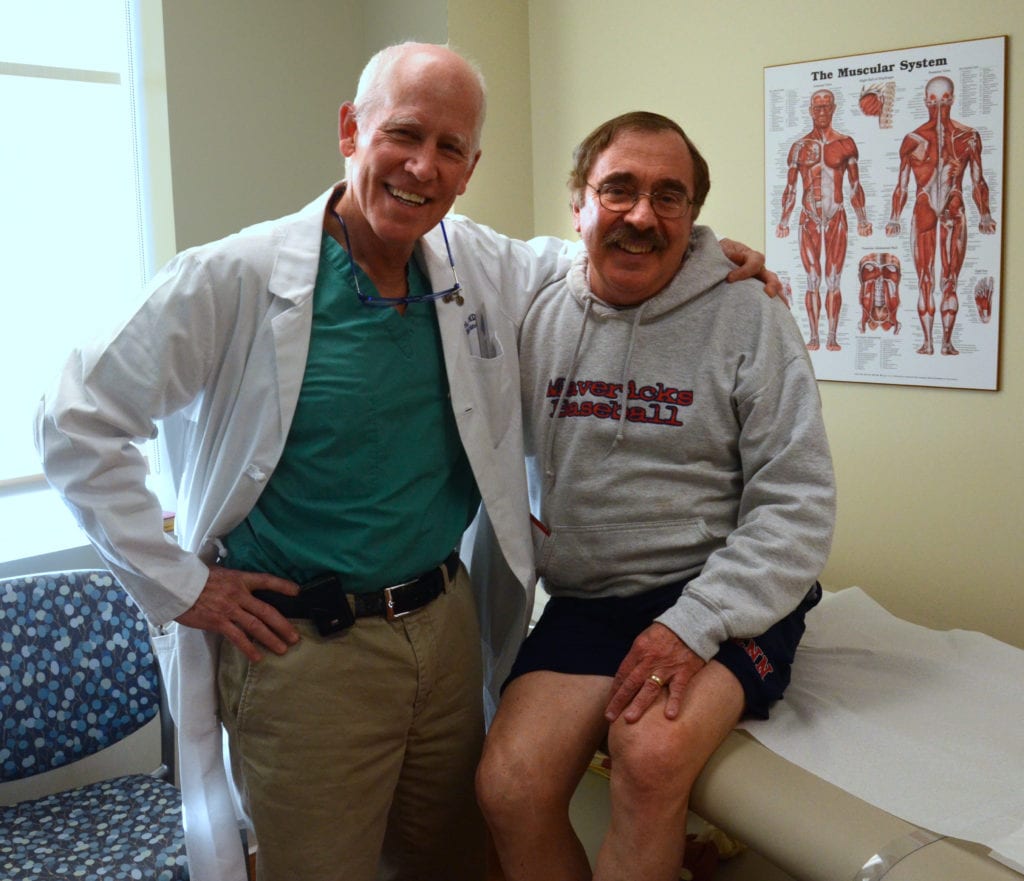
Below is our Q&A with Dr. Noerdlinger, an orthopedic surgeon specializing in the shoulder. Dr. Noerdlinger is a partner at Atlantic Orthopaedics with extensive experience performing the Stryker InSpace Balloon procedure.
Q: In your own words, how does this procedure benefit your patients?
A: This is a pain relieving procedure.
Q: Who is a good candidate for the Stryker InSpace Balloon procedure?
A: The procedure is indicated for patients with irreparable rotator cuff tears, with good shoulder function and minimal to no arthritis.
Q: Where do you perform this procedure?
A: I perform the procedure at NECOS (New England Center for Orthopaedic Surgery) in Portsmouth, and York Hospital in Maine.
Q: Do you have a recent patient success story you can share?
A: I performed the Stryker InSpace Balloon procedure on a 67 year old man with years of pain and an unfixable rotator cuff tear. He described his shoulder as getting worse despite physical therapy and injections. He had pain with an active range of motion, and stated his shoulder was 30% normal. Four months after his February surgery, he described his pain as a 2 out of 10 on a daily basis and rated his shoulder as 60% normal.
I also treated a 73 year old female patient who came to me with pain from an irreparable rotator cuff tear. She described her shoulder as 40% normal before the procedure and 70% normal 3 months after her March 1st surgery.
Another patient, a 60 year old man with bilateral irreparable rotator cuff tears, had the balloon placed in his right shoulder on March 1st, and his shoulder improved from 20% normal to 65% normal in 6 weeks. He then underwent left shoulder balloon placement May 10th.
Q: Anything else you’d like current or future patients to know about this procedure and how it would benefit them?
A: The rotator cuff is the one structure that, when torn, causes the most pain and dysfunction in the shoulder. Rotator cuff tears do not heal, get bigger over time, become unfixable, and cause arthritis. Rotator cuff repair surgery is very successful and can restore normal, pain-free function.
If the rotator cuff is irreparable, the painful shoulder is often treated with a reverse shoulder replacement. For patients with unfixable, painful rotator cuff tears with little to no arthritis and good function, an InSpace balloon is a good option.
If you’re suffering from shoulder pain from a rotator cuff tear that hasn’t responded to treatments like injections or physical therapy, schedule an appointment to find out if the Stryker InSpace Balloon procedure is right for you.